Does Stress Cause IBS?
Many people with irritable bowel syndrome (IBS) have been told that if they could just stop worrying, their IBS would be cured. While this is definitely NOT true, we are learning that stress and IBS symptoms may be linked in some very interesting ways.
The gut-brain connection
If you have IBS, you may have found that stress can trigger your IBS symptoms. But did you know that your gut may actually influence your emotions?
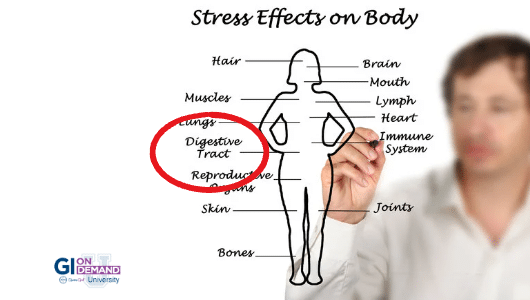
Researchers have been studying what’s called the “gut-brain connection” and have found that the nerves along our digestive tract can influence our brains. Their studies suggest that irritation in the gastrointestinal system can trigger mood changes and may lead to the anxiety and depression that can accompany IBS.
This growing understanding of the relationship between the gut and the brain has opened the door for therapies that target both the brain and the gut.
Healthy brain = healthy gut?
Since our brain and our gut “talk” to each other, it’s important to keep those lines of communication open.
Cognitive behavioral therapy (CBT) for IBS is one treatment tool that can help support the connection between the gut and the brain. CBT is a type of psychotherapy that involves working with a mental health counselor to help change the way you think and respond to stress.
Another therapy that may help facilitate the gut-brain connection is prescription antidepressants. If your gastroenterologist recommends antidepressants, it’s not because they think that your IBS is all in your head, it’s because these medicines can act on the nerve cells in the gut and help with IBS symptoms.
Aside from therapy and medications, there are also lifestyle changes that you can make to lower stress and support the communication between your gut and your brain.
5 ways to support your gut-brain connection
1. Symptom journaling
Getting in touch with your IBS symptoms can be a great first step towards managing them.
Check in with yourself at the beginning or end of each day and make a few notes about your IBS symptoms. Did you feel more or less bloated than usual? How many bowel movements did you have that day?
It may feel a little strange at first, but taking note of your daily symptoms can help you draw connections between your symptoms and your habits and can help you track your improvement.
2. Yoga
Yoga is a fantastic tool for IBS management that may help reduce symptoms and improve quality of life, according to research.
Learning the basics of yoga from a yoga class or instructional video is a good way to start. Then you can either jump-start your day with morning yoga or use it to unwind when you get home from work (or both!).
3. Mindful eating
Mindful eating is a skill that can help you prepare your body for a meal. It can be used anytime, but can be especially helpful if you are reintroducing foods or trialing new foods.
The practice of mindful eating involves getting into a quiet place to eat, thinking about how the food you are about to eat will nourish you and not cause you symptoms, and then slowly eating while staying mindful and enjoying each bite.
It takes time and lots of practice to become a mindful eater, but working with an experienced registered dietitian can help you get there.
4. Gratitude
When you have IBS, it can feel like everything in the world is against you. Starting a daily gratitude practice can help you break out of those negative thoughts and start focusing on what you are grateful for. Many people use a gratitude journal, but you can also practice gratitude during yoga or other forms of movement.
5. Daily movement
While not all types of movements are best for IBS, gentle activities that do not trigger your symptoms can go a long way towards lowering stress and supporting your gut-brain connection.
Activities like walking, biking, and swimming are all great options.
While stress alone does not cause IBS, it’s becoming more clear that there is an important relationship between the gut and the brain. There are plenty of ways to help support this gut-brain connection and these practices may be important tools for your unique IBS management plan.
Katelyn Collins, RD is a registered dietitian specializing in irritable bowel syndrome (IBS) and digestive health. Katelyn’s personal experience with IBS first sparked her passion for nutrition and health. Since then, she has been a vocal advocate for the digestive health community and has dedicated her own nutrition practice to serving those with digestive conditions.
Listen to our
latest Podcast!