Jacqueline A. Gaulin
Founder, Chief Strategy Officer
Jacqueline Gaulin is the Founder and Chief Strategy Officer of Gastro Girl, Inc. She created the concept of Gastro Girl based upon her passion for helping individuals with digestive health issues and the role the gastrointestinal tract has on overall health and wellness. She is a certified health coach and was previously the Director of Communications and Digital Engagement for the American College of Gastroenterology.

Health Hub
 Diarrhea
Diarrhea
 Eosinophilic Esophagitis
Eosinophilic Esophagitis
 Poop
Poop
 IBS-C
IBS-C
 IBS
IBS
 Irritable Bowel Syndrome
Irritable Bowel Syndrome
 Abdominal Pain
Abdominal Pain
 Appendicitis
Appendicitis
SELECT A TOPIC!

Latest Blog Articles
A collection of helpful articles curated and written by Gastro Girl.
October 22, 2025
Hemorrhoids: Symptoms, Treatment, Prevention
August 19, 2025
Struggling to Swallow: My EoE Journey
August 22, 2024
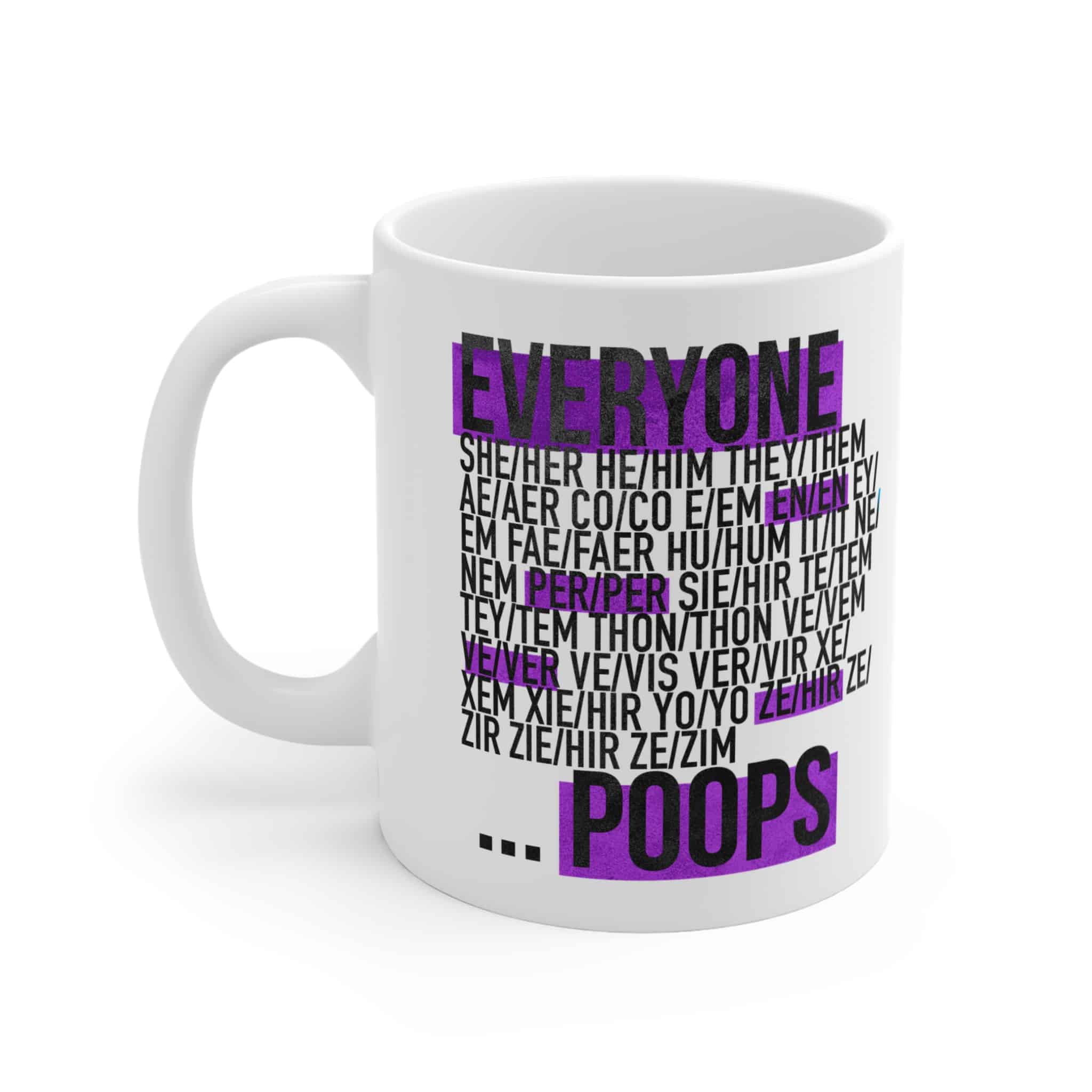
Merch Drop!
The Gastro Girl Team is super excited to share our very first Merch Drop! Please check out our debut collection and let us know what you think! Your purchases support our patient-centric efforts to provide evidence-based digestive health education, content, access to expertise and support for everyone. Thank you!
April 1, 2023
Tips for Providing Care to Older Adults with Digestive Issues
Digestive conditions can make caregiving seem daunting, so we’ve put together a few tips to make the situation easier for both you and your loved one!
March 30, 2021
The Who, What, Why, and How of Colorectal Cancer Screening
We are taking action all month long to help promote the importance of colorectal cancer screening. Read on to learn more about screening and find out how to get involved with helping to spread awareness!
February 22, 2021
3 Tips for Caregivers During COVID-19
Caregivers are the unsung heroes of the COVID-19 pandemic. As if being a caregiver isn’t hard enough, you now have the added challenges that come with caregiving during a pandemic. To help support you during this difficult time, we’ve put together our top tips for coping with the struggles of caregiving during the pandemic.
October 22, 2025
Hemorrhoids: Symptoms, Treatment, Prevention
August 19, 2025
Struggling to Swallow: My EoE Journey
February 28, 2025
Article: Q&A: AI-powered app ‘digestive health companion’ empowers patients to improve gut health
Click here to read an article published by Healio about the Ask Gastro Girl App.
February 12, 2025
Article: Building a Repository of Answers to All Your Digestive Health Queries
Click here to read an article published by Medhealth Outlook about the Ask Gastro Girl App.
January 16, 2025
Gastro Girl Unveils ‘Ask Gastro Girl’: The AI-Powered App Redefining Access to Digestive Health Support
Startup life is relentless. The challenges are overwhelming, the sacrifices endless, and at times, the vision you’re fighting for can feel distant. But for me, that vision has always been about bold thinking—challenging the status quo and empowering people to take control of their digestive health.
January 3, 2025
Ask Gastro Girl App: AI-Powered Support for Gut Health
Startup life is relentless. The challenges are overwhelming, the sacrifices endless, and at times, the vision you’re fighting for can feel distant. But for me, that vision has always been about bold thinking—challenging the status quo and empowering people to take control of their digestive health.
August 19, 2025
Struggling to Swallow: My EoE Journey
May 12, 2025
Shining a Light on EoE: Stories, Support, and Hope
In honor of the first World Eosinophilic Esophagitis (EoE) Day on May 22, 2025, Gastro Girl is helping to shine a spotlight on this chronic and progressive disease all month long—with stories, support, and resources that remind us why awareness matters.
Introducing the Gastro Girl Podcast!
If you’re one of the 1 in 4 people who is living with a chronic digestive health condition , you’re not alone. Whether you’re just diagnosed, in remission, or trying to learn what is happening in your body and what you can do about it, then this podcast is for you.
February 13, 2026
Barrett’s Esophagus in the U.S.: How GERD Increases Cancer Risk
Chronic heartburn and GERD are often brushed off as everyday issues—but for some patients, long-term reflux can quietly progress to Barrett’s esophagus, the only known precursor to esophageal cancer. In Part 1 of this 4-part U.S.-focused patient education series, foregut surgeon Dr. Dan Lister, Founder of the Arkansas Heartburn Treatment Center, explains how reflux disease can evolve over time and why early recognition matters. In this episode, you’ll learn: – How chronic GERD can progress silently – Why Barrett’s esophagus matters—even when symptoms improve or disappear – Key warning signs patients should never ignore – How Barrett’s is detected and risk is assessed in the U.S. – Treatment approaches that may help reduce cancer risk Whether you’ve lived with reflux for years or are newly diagnosed, this episode provides clear, evidence-based guidance to help you take reflux seriously—and take action. This episode is part of a 4-part patient education series sponsored by Castle Biosciences and produced in collaboration with leading U.S. clinicians dedicated to improving outcomes for patients with Barrett’s esophagus.
January 14, 2026
MASH Explained: Symptoms, Diagnosis, Testing, and What Patients Need to Know
MASH—metabolic dysfunction–associated steatohepatitis (formerly known as NASH)—is a progressive form of fatty liver disease that often develops silently, without obvious symptoms. Many people don’t realize their liver is being damaged until the disease has already advanced. In this episode of the Gastro Girl Podcast, host Jacqueline Gaulin is joined by Dr. Pooja Singhal, a board-certified gastroenterologist, hepatologist, obesity medicine specialist, and founder of the Oklahoma Gastro Health and Wellness Center. Dr. Singhal explains: – The difference between MASLD and MASH – Why MASH is frequently missed or diagnosed late – Why testing—not symptoms—is the only reliable way to assess liver health – Who is at risk for developing MASH – How MASH is diagnosed and what liver testing involves – Why fibrosis (liver scarring) matters – Current treatment, prevention, and long-term management strategies – How early identification can help reduce the risk of cirrhosis and liver cancer This episode focuses specifically on MASH, the progressive form of fatty liver disease. MASLD is discussed only to help listeners understand how MASH develops and why timely testing matters. Designed to reduce confusion, raise awareness, and empower patients, this conversation equips listeners with the knowledge they need to have informed discussions with their healthcare providers. Thank you to Madrigal Pharmaceuticals for supporting this episode.
December 16, 2025
Understanding Fecal Incontinence in Adults: What Patients Need to Know
Fecal incontinence (FI) affects nearly 8% of adults worldwide, yet many people suffer in silence due to embarrassment, confusion, or the belief that nothing can be done. This episode aims to change that. We’re joined by Dr. John William Blackett, gastroenterologist and lead author of the recent article “Fecal Incontinence in Adults: New Therapies,” published in The American Journal of Gastroenterology. Dr. Blackett shares a compassionate, patient-centered perspective on FI—covering common causes, diagnostic testing, and the full spectrum of treatment options available today, including newer therapies. If you’ve experienced unexpected leakage, urgency, staining, or difficulty controlling bowel movements—or if you support someone who has—this episode offers clarity, hope, and practical guidance. Effective treatments exist, and help is available. This episode is produced in collaboration with the American College of Gastroenterology Patient Care Committee.

Video Gallery
February 13, 2026
Barrett’s Esophagus in the U.S.: How GERD Increases Cancer Risk
Chronic heartburn and GERD are often brushed off as everyday issues—but for some patients, long-term reflux can quietly progress to Barrett’s esophagus, the only known precursor to esophageal cancer. In Part 1 of this 4-part U.S.-focused patient education series, foregut surgeon Dr. Dan Lister, Founder of the Arkansas Heartburn Treatment Center, explains how reflux disease can evolve over time and why early recognition matters. In this episode, you’ll learn: – How chronic GERD can progress silently – Why Barrett’s esophagus matters—even when symptoms improve or disappear – Key warning signs patients should never ignore – How Barrett’s is detected and risk is assessed in the U.S. – Treatment approaches that may help reduce cancer risk Whether you’ve lived with reflux for years or are newly diagnosed, this episode provides clear, evidence-based guidance to help you take reflux seriously—and take action. This episode is part of a 4-part patient education series sponsored by Castle Biosciences and produced in collaboration with leading U.S. clinicians dedicated to improving outcomes for patients with Barrett’s esophagus.
January 14, 2026
MASH Explained: Symptoms, Diagnosis, Testing, and What Patients Need to Know
MASH—metabolic dysfunction–associated steatohepatitis (formerly known as NASH)—is a progressive form of fatty liver disease that often develops silently, without obvious symptoms. Many people don’t realize their liver is being damaged until the disease has already advanced. In this episode of the Gastro Girl Podcast, host Jacqueline Gaulin is joined by Dr. Pooja Singhal, a board-certified gastroenterologist, hepatologist, obesity medicine specialist, and founder of the Oklahoma Gastro Health and Wellness Center. Dr. Singhal explains: – The difference between MASLD and MASH – Why MASH is frequently missed or diagnosed late – Why testing—not symptoms—is the only reliable way to assess liver health – Who is at risk for developing MASH – How MASH is diagnosed and what liver testing involves – Why fibrosis (liver scarring) matters – Current treatment, prevention, and long-term management strategies – How early identification can help reduce the risk of cirrhosis and liver cancer This episode focuses specifically on MASH, the progressive form of fatty liver disease. MASLD is discussed only to help listeners understand how MASH develops and why timely testing matters. Designed to reduce confusion, raise awareness, and empower patients, this conversation equips listeners with the knowledge they need to have informed discussions with their healthcare providers. Thank you to Madrigal Pharmaceuticals for supporting this episode.
Gastro Girl’s Favorite Things
Gastro Girl Canvas Tote Bag
Lightweight and durable—this polyester canvas tote bag does it all. The inside has a sleek, black lining and its comfortable[…]
Gastro Girl Unisex Hooded Sweatshirt
Made to be stylish as well as comfortable, the Independent Trading Co. personalized hooded sweatshirt delivers on all fronts. Made[…]
“Everyone Poops” Mug (11oz)
Perfect for coffee, tea and hot chocolate, this classic shape white, durable ceramic mug comes in the most popular size.
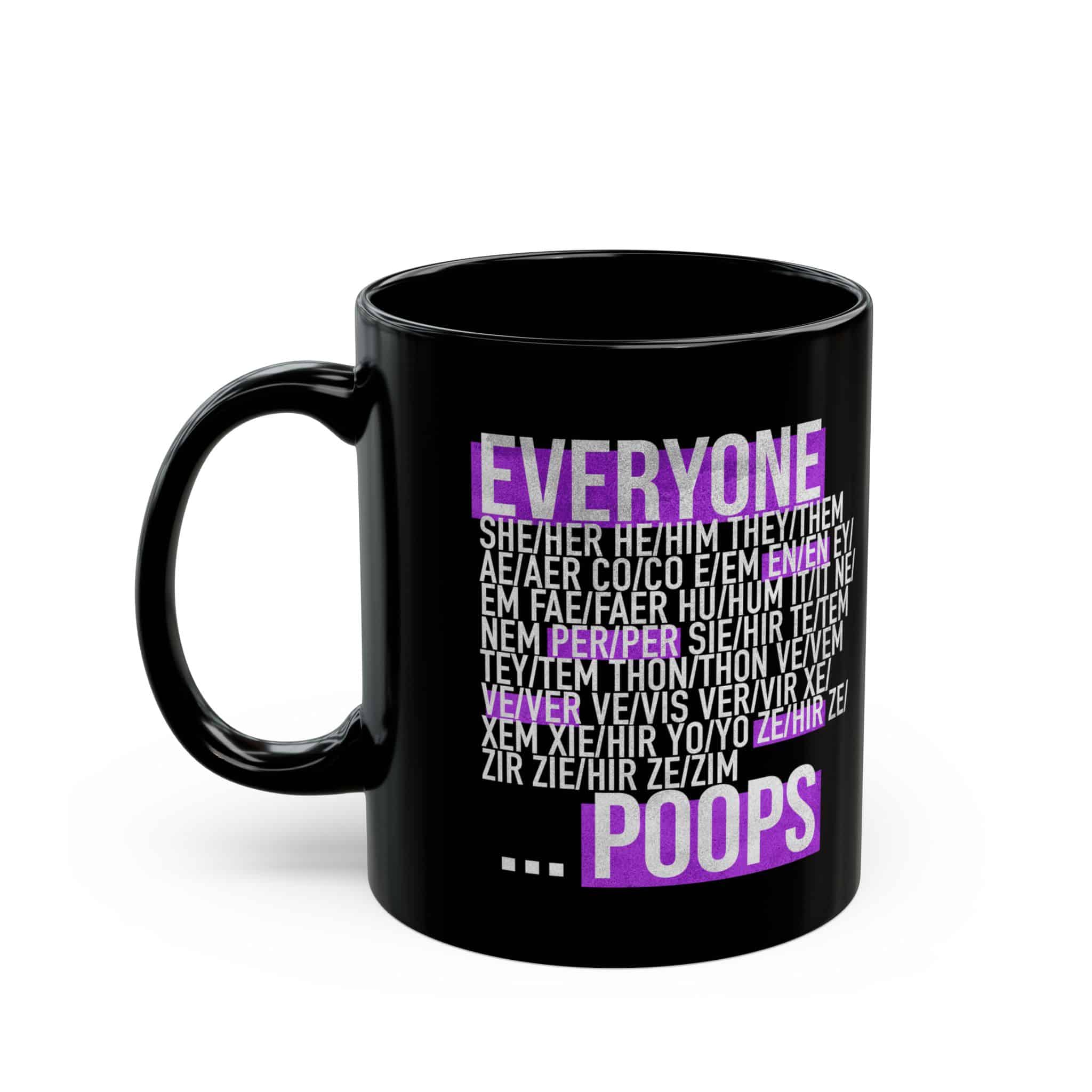
“Everyone Poops” Black Mug (11oz)
Warm your soul with a nice cuppa out of this black ceramic mug. It’s BPA and lead-free, microwave and dishwasher-safe,[…]

Contact Us
Use this form to get in touch with us!
"*" indicates required fields