What You Should Know About Constipation
Let’s face it, constipation is uncomfortable. Constipation not only causes physical discomfort, but it can also be uncomfortable to talk about. Some people deal with chronic constipation for years and never seek help.
To help get the conversation on constipation going, we recently had the pleasure of speaking with Dr. Darren M. Brenner on the Gastro Girl Podcast. Dr. Brenner is a gastroenterologist, motility expert, and co-author of a recent review article which looked at over-the-counter treatments for constipation.
Read on for more information about the symptoms and causes of constipation, and learn what you can do about it!
What is constipation?
In general, a person has constipation if their bowel movements become less frequent and difficult to pass. Stools (AKA poop) can be hard and dry and there can be a feeling of incomplete emptying of the bowels.
Dr. Brenner tells us that constipation is classified as a functional gastrointestinal disorder and it is different from irritable bowel syndrome with constipation (IBS-C). In IBS-C, there is abdominal pain, discomfort, abdominal distention, and bloating.
How common is constipation?
According to Dr. Brenner, the definition of constipation can vary between patients and doctors. He says that many people think they have constipation if they do not have a daily bowel movement, but the normal range is actually “three times a day to three times a week.”
Since definitions of constipation can vary widely, it’s hard to pinpoint the prevalence rates. Dr. Brenner tells us that if strict criteria are used, “the prevalence of constipation in the United States is about 7% and internationally it’s about 12%”.
Causes of constipation
Dr. Brenner breaks down the causes of constipation into three main categories:
1. Motility Issue
When the digestive tract is working properly, the muscles stretch and contract to move food along. According to Dr. Brenner, when someone has a problem with their gut motility, “things don’t move through the GI tract fast enough.”
2. Brain-Gut Visceral Perception Issue
Brain-gut visceral perception is the way we feel sensations in our digestive system. Dr. Brenner tells us that when someone has a visceral perception issue, “the stuff moves down the GI tract just fine, but they feel like they are straining too much and they don’t feel like they get everything out.”
3. Pelvic Floor Issue
The pelvic floor is a group of muscles that play a role in having a bowel movement.
When issues with the pelvic floor cause constipation, “the stool gets down to the bottom, but the muscles that we have in the bottom that we need to relax to allow the stool to come out don’t work right,” says Dr. Brenner. Furthermore, if the pelvic floor is the cause of constipation, then laxatives will not be the proper treatment.
Another very important point that Dr. Brenner reminds us of is the connection between constipation and a history of trauma or abuse. He says that it’s essential for practitioners to become more aware of this.
Constipation treatments
Dr. Brenner tells us that there are a wide variety of treatments and therapies being used for constipation, but it’s important to understand how effective each one is and when they should be used.
Over-the-counter constipation treatments
The recent article that Dr. Brenner co-authored provides a detailed review of the research behind different types of over-the-counter (OTC) laxatives.
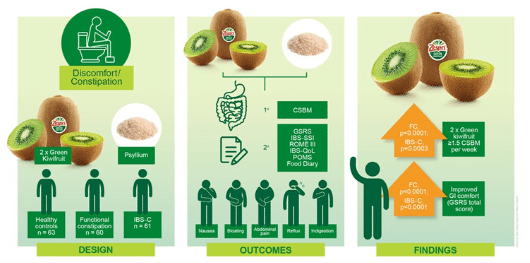
The list includes osmotic laxatives (like MiraLAX® ) which draw fluid into the intestine to make stools softer and increase the movement of the intestines. There are also stimulant laxatives (like senna) and fiber supplements (like psyllium husk).
According to Dr. Brenner, there have not been any clinical trials showing the benefits of magnesium-containing agents or stool softeners, although these products are widely used.
Prescription treatments
OTC laxatives are often the first line of treatment that Dr. Brenner recommends for constipation, but the decision to use prescription treatments will depend on symptoms.
“There is really little to no data suggesting that over-the-counter treatments can improve abdominal symptoms,” says Dr. Brenner. This means that if a patient has symptoms of IBS-C, such as pain and bloating, he will consider using a prescription because OTC treatments will likely not help with these symptoms.
Nutrition and exercise
There are certain foods that have been shown to be beneficial for constipation. According to Dr. Brenner, kiwi fruits, mangos, and prunes may help.
But what about foods to avoid?
Dr. Brenner says that “when we talk about constipating foods, there’s not a lot of data out there to suggest that one particular food over another one is going to increase your risk of developing constipation.”
While many people are told to drink more water and get more exercise to deal with constipation, Dr. Brenner tells us that there is no data to show that drinking more water can help. But he does mention that exercise may help get things moving.
Pelvic floor physical therapy
If pelvic floor issues are the cause of constipation, seeing a pelvic floor physical therapist can be helpful. Dr. Brenner recommends to start looking into this if you’ve tried at least two evidenced-based treatments and are still having symptoms.
When to seek help for constipation
“Trying a couple over-the-counter therapeutics is okay before you talk to a practitioner,” says Dr. Brenner. If you are using multiple laxatives, or increasing the doses, it’s time to see a doctor.
If you have been working with a practitioner for a while and you are still having symptoms, Dr. Brenner recommends asking if pelvic floor issues may be the cause.
As Dr. Brenner says, constipation “is not a one-size-fits-all disorder.” Empowering yourself with knowledge about the treatment of constipation can help you find relief and give you the tools you need to ask for help!
References:
Rao, S., & Brenner, D. M. (2021). Efficacy and Safety of Over-the-Counter Therapies for Chronic Constipation: An Updated Systematic Review. The American journal of gastroenterology, 116(6), 1156–1181. https://doi.org/10.14309/ajg.0000000000001222
Listen to our
latest Podcast!