Personalized Diet, Education Program Yield Weight Loss, Improve GERD in Obese Patients
Obese patients who received a personalized diet program and multidisciplinary education had improvements in gastroesophageal reflux (GERD) symptoms, weight loss and better quality of life, according to the results of a study published in The American Journal of Gastroenterology’s “Putting Patients First” special issue. The “Putting Patients First” issue includes studies using patient-reported outcomes and highlights patients’ experiences with their disease.
Obesity is an important independent risk factor for gastroesophageal reflux disease (GERD) (1, 2). In observational studies and systematic reviews, weight loss is reported as one of the few effective lifestyle modifications for GERD (1, 3, 4). Yet, current health care systems do not effectively promote weight reduction in patients with obesity and GERD, according to researchers from the division of gastroenterology and hepatology at the University of Colorado Anschutz Medical Campus. They designed The Reflux Improvement and Monitoring (TRIM) program specifically to treat patients with obesity and GERD. The six-month TRIM program consisted of an initial consultation followed by 3 weekly sessions and then 5 monthly sessions. The initial consultation included a baseline weigh-in, standardized education, personalized goal-setting, weekly meal planning and instructions on how to use nutrition tracking tools. Educators reviewed these goals and reinforced lessons at the ensuing follow-up sessions, according to the study.
“Through the focus groups we uncovered that many patients were unaware of and did not independently recognize the link between weight and GERD before TRIM participation”, according to investigators. “Yet, patients shared a strong desire to alleviate symptoms and reduce PPI use. Results from our mixed methods study suggest that weight loss becomes a more desirable and attainable goal once patients associate weight loss with symptom relief, further underscoring the value of health education. The idea that symptom relief is a powerful facilitator of healthy behaviors is intriguing and likely transcends symptom-based disorders across medicine,” they wrote in the study.
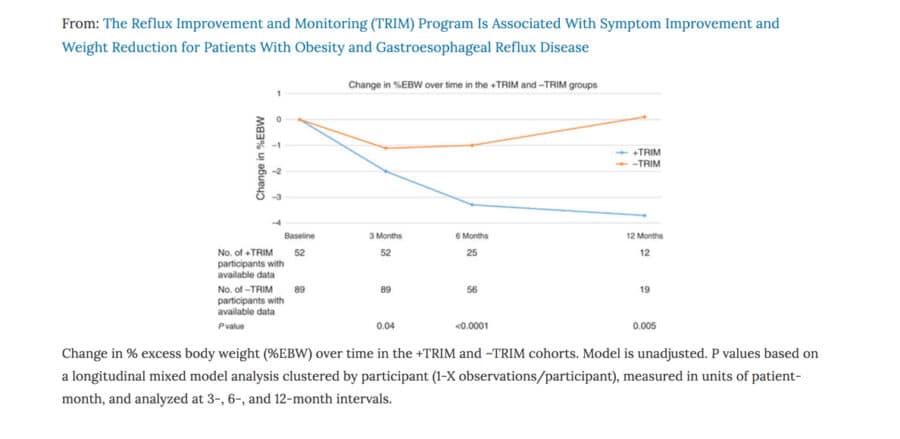
While this feasibilty study had some inherent limitations, which included losing some participants to follow-up, this prospective mixed methods feasibility study highlights the positive effects of TRIM including:
- Patients participating in TRIM had significant symptom reduction and when compared with patients not participating in TRIM, significant weight loss.
- Strengths of TRIM include optimized EHR functionality, minimal interference with clinician workflow, multidisciplinary care coordination, and a patient-centered approach.
- Lifestyle management programs tailored to patients with obesity and with GERD, such as TRIM, should be integrated into health promotion practices.
References
1. Park SK, Lee T, Yang HJ et al. Weight loss and waist reduction is associated with improvement in gastroesophageal disease reflux symptoms: a longitudinal study of 15 295 subjects undergoing health checkups. Neurogastroenterol Motil 2017;29 doi: 10.1111/nmo.13009 (e-pub ahead of print 21 December2016).
2. El-Serag HB, Graham DY, Satia JA et al. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol 2005;100:1243–1250
3. Ness-Jensen E, Hveem K, El-Serag H et al. Lifestyle intervention in gastroesophageal reflux disease. Clin Gastroenterol Hepatol 2016;14:175–182 e1-3.
4. de Bortoli N, Guidi G, Martinucci I et al. Voluntary and controlled weight loss can reduce symptoms and proton pump inhibitor use and dosage in patients with gastroesophageal reflux disease: a comparative study. Dis Esophagus 2016;29:197–204.
Related Resources
The Reflux Improvement and Monitoring (TRIM) Program Is Associated With Symptom Improvement and Weight Reduction for Patients With Obesity and Gastroesophageal Reflux Disease, The American Journal of Gastroenterology Volume 113, pages 23–30 (2018) doi:10.1038/ajg.2017.262
Listen to our
latest Podcast!