Proton Pump Inhibitors (PPIs) and COVID-19 Risk: What You Need to Know
On July 7th, 2020, The American Journal of Gastroenterology released the following study examining the relationship between use of PPIs and risk of COVID-19: “Increased risk of COVID-19 among users of proton pump inhibitors” Am J Gastroenterol 2020 (pre-print posted online July 7, 2020) Authors: Almario CV, Chey WD, Spiegel BMR.
In this document, members of the American College of Gastroenterology (ACG) leadership team partnered with the study authors to prepare a brief overview of the research, discuss its findings, and address potential implications for clinical care. The full study in pre-print format can be found at this link.
Here are some key take-aways that patients can use
to discuss this study with their healthcare provider:
What are the main results of the study?
This study was an online population-based survey of 53,130 English-speaking adult Americans. Respondents were asked about any current PPI and/or histamine-2 receptor antagonist (H2RA) use and were also asked about whether they have tested positive for COVID-19. The authors then performed a regression analysis to test the relationship between anti-secretory use and risk of COVID-19 while adjusting for a wide range of potential confounders, including demographic, socioeconomic, lifestyle, and comorbidity variables.
- The authors found that PPI use was independently associated with increased odds for COVID-19.
- Moreover, there was a dose-response relationship between the amount of acid suppression and the risk of COVID-19 that fell along a biological gradient. Compared to those not using PPIs, those taking twice-daily PPIs registered a 3.7-fold increased odds of COVID-19, whereas those using PPIs up to once daily had a 2.2-fold increase. In contrast, people taking less powerful H2RAs were not at increased risk for COVID-19.
- Of note, the risk of PPIs remained significant regardless of duration of use, including those who had been on PPIs for six months or greater, before the start of the pandemic.
- In addition to PPI usage, males, current smokers, non-Hispanic blacks, and Latinxs were significantly more likely to report being positive for COVID-19, consistent with previous research.Do patients need to stop their PPIs right now because of this study? As always, the decision about whether, when, and how to modify PPIs dosing should be based on a thoughtful assessment of the risk-benefit ratio for individual patients.
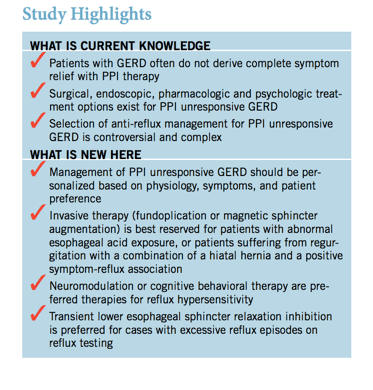
This study does not definitively prove that PPIs increase the risk for COVID-19. As with any medication, the lowest effective dose should be used when clinically indicated, and, when appropriate and consistent with best-practice guidelines, H2RAs may also be considered as an alternative treatment for acid-related conditions.
Do patients need to stop their PPIs right now because of this study?
As always, the decision about whether, when, and how to modify PPIs dosing should be based on a thoughtful assessment of the risk-benefit ratio for individual patients. This study does not definitively prove that PPIs increase the risk for COVID-19. As with any medication, the lowest effective dose should be used when clinically indicated, and, when appropriate and consistent with best-practice guidelines, H2RAs may also be considered as an alternative treatment for acid-related conditions
What else do patients need to know?
- The main result of this study is that use of PPIs, particularly twice-daily PPIs, appears to increase the risk of COVID-19. Although the relative risk is notable, with an adjusted odds ratio of 3.7 for twice-daily dosing, the absolute risk is still small for any individual patient using PPIs.
- For patients using PPIs for an appropriate indication who are concerned about COVID-19, the best way to reduce personal risk is to practice regular hand washing, practice social distancing, and wear a mask when around others.
- These practices will have a much greater impact on personal risk of COVID-19 than manipulating PPI dosing.
- If nothing else, the discussion about PPI risk could save lives simply by reminding users to closely adhere with CDC guidelines given the potentialincreased risk conferred by PPIs.
- Beyond the critical point of emphasizing adherence with CDC guidelines, patients should ask their doctor if twice-daily PPI dosing is necessary for them, particularly those who are especially vulnerable for severe COVID-19 (e.g., elderly or comorbid patients). Although individual patients may certainly benefit from twice-daily dosing, it is always useful to re-evaluate the need for high-dose PPIs, particularly during a pandemic when the population prevalence of COVID-19 remains high.It is important to emphasize that this study extends upon previously published research: that PPIs increase the risk of gastrointestinal infection.
- Although the absolute risk of any PPI-induced infection is low, previous research has shown a clear link between PPI use and an increased odds of gastrointestinal infections.4- 6 The current study’s novelty lies in the extension of this knowledge to COVID-19. It is reasonable to make sure there is a clear indication in all patients taking a PPI. When a PPI is indicated, clinicians should inform their patients about the association betweenPPIs and enteric infections, now including COVID-19, just as it would be useful to review potential side effects whenever prescribing any other medicine.
- The benefits and risks of PPI therapy should be carefully considered and balanced to arrive at an individualized decision for each individual patient.
Bottom line: It is important to speak with your doctor or other healthcare provider about this study and your related concerns and questions to determine the best treatment option for your individual health condition or situation.
Listen to our
latest Podcast!