6 IBS Myths Debunked by a Gastroenterologist
IBS can often be a misunderstood condition, so we invited Brian Lacy, PhD, MD, FACG on our podcast to provide his expert knowledge on all-things IBS.
As a gastroenterologist and professor of medicine at the Mayo Clinic in Jacksonville, Florida, Dr. Lacy brings a combination of evidence-based insights and clinical experience to the conversation.
Using the information provided by Dr. Lacy and other research-backed resources, we put together a reference on common IBS Myths and Facts just for you!
Myth #1: IBS is all in your head
While the brain does play a role in IBS symptoms, it’s important to understand that IBS is a real condition that goes beyond a single psychological cause. Years ago, many people with IBS were dismissed as being depressed or hysterical. But we now know that this is simply untrue.
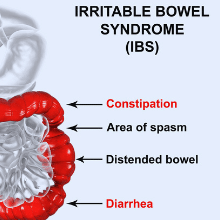
According to Dr. Lacy, IBS is a “disorder of gut-brain interaction” which means “that you have lots of signals going between the gut and the brain and the brain and the gut.” A disorder in this “bidirectional pathway” of communication between the gut and brain can lead to IBS symptoms such as abdominal pain, bloating, diarrhea, and/or constipation.
Dr. Lacy tells us that those with IBS “may sense pain differently in their brain or react to pain differently.” The gut and brain are supposed to talk to each other, but the volume on this conversation is turned up too high.
You can learn more about the gut-brain connection in GI conditions from our podcast episode with GI health psychologist, Dr. Megan Riehl.
Myth #2: IBS can turn into a more serious condition
When a person first gets diagnosed with IBS, they may initially be relieved to learn that they do not have a life-threatening disease. However, some people then incorrectly think that their IBS is going to inevitably lead to something more serious.
Dr. Lacy says that a survey study found that “about 30% of people with IBS were convinced that it was going to turn to cancer” and “about 25% of people are convinced that IBS turns to IBD [or inflammatory bowel disease].”
Thankfully, neither of these assumptions are true! Dr. Lacy says that IBS does not turn into IBD or cancer, and it does not decrease life expectancy.
These misconceptions further highlight why it’s so important to share accurate information about IBS!
Myth #3: IBS is a rare condition
Even though IBS can feel isolating, it’s actually more common than many people think.
Dr. Lacy explains that IBS “affects anywhere from about 1 in 10 to 1 in 20 adult Americans.” While anyone can have IBS, he also tells us that it’s a little more common for people in their mid-20’s to mid-40’s.
If you’re feeling alone in your struggles with IBS, we encourage you to join the GI OnDEMAND Patient Education Community and talk to your gastroenterologist about support groups offered through their practice.
Myth #4: Only women get IBS
Contrary to popular belief, men have IBS too!
According to Dr. Lacy, IBS is a little bit more common in women, but he emphasizes that the difference in rates is much smaller than most people think.
There does seem to be a difference between men and women when it comes to IBS symptoms. Men are “a little bit more likely to have IBS with diarrhea symptoms, as opposed to women [who are] a little bit more likely to have IBS with constipation symptoms”, says Dr. Lacy.
Myth #5: There is a simple test for IBS
There is no single test for IBS at this time.
Dr. Lacy explains that physicians use the Rome IV criteria to diagnose IBS. “We ask about those classic symptoms”, says Dr. Lacy, which include abdominal pain and bloating. They will also ask about disordered bowel habits such as diarrhea, constipation, or a combination of both.
Dr. Lacy tells us that in addition to taking a detailed history and performing a physical exam, physicians will also look for warning signs of serious conditions in order to rule them out.
Myth #6: There is no treatment for IBS
There are actually a variety of evidence-based treatment options available for those with IBS!
Dr. Lacy is the first author on the latest ACG Clinical Guideline for the Management of Irritable Bowel Syndrome. The guideline provides a review of the available treatments for IBS and serves as a tool for physicians and gastroenterologists.
It’s important to work with your healthcare provider on a comprehensive treatment plan for your IBS. Dr. Lacy suggests including lifestyle changes in this plan that cover diet, exercise, sleep, and stress reduction. He also recommends working with a registered dietitian on dietary changes for IBS symptom management.
Once you have a treatment plan in place, IBS can feel much more manageable!
If you still have questions about IBS treatment for yourself or a loved one, we encourage you to check out Making Sense of IBS: A Physician Answers Your Questions about Irritable Bowel Syndrome by Dr. Brian Lacy.
Resources
April 20, 2022
What You Need to Know About IBS
Are you living with chronic digestive health issues like bloating, constipation, gas? Are you unsure of how to talk to your doctor about these symptoms? In honor of IBS Awareness Month Dr. Brian Lacy, a gastroenterologist at the Mayo Clinic in Jacksonville, FL, provides insight on the symptoms, diagnosis, treatment, and common misperceptions about IBS and offers tips for talking with your doctor about these potentially embarrassing symptoms.
April 20, 2022
What Comes First, The Gut or The Brain?
Dr. Megan Riehl is a GI Health Psychologist with the University of Michigan and Director of Behavioral Health Services for Gastro Girl and GI OnDEMAND. In today’s interview, Dr. Riehl breaks down the concept of the “gut-brain connection”. She explains that our gut and brain are supposed to talk to each other, but the volume on this conversation is turned up too high for those with GI conditions. Dr. Riehl then puts on her Gastro Psych hat for us and provides actionable tips for finding peace during these difficult times.
April 20, 2022
IBS: It’s Not All In Her Head, Or His
Is IBS different for men and women? Why is it more common for women to be diagnosed? Are men suffering in silence? We get to the bottom of these questions and more with two longtime IBS patient advocates, Johannah Ruddy, Executive Director of the Rome Foundation, and Jeffrey Roberts, founder of ibspatient.org. Johannah and Jeffrey share their unique perspectives on living with IBS, how men and women may approach their symptoms differently, and why the brain-gut connection is key to understanding IBS.
April 20, 2022
How Do I Talk to My Doctor About My IBS and IBS with Constipation Symptoms and Treatment Options?
Open communication between patients and their health care providers is vital for accurate and timely diagnosis and treatment, especially for GI conditions like Irritable Bowel Syndrome (IBS) or IBS with Constipation (IBS-C), which often present with multiple symptoms and are impacted by lifestyle factors like diet and stress. In this episode, Dr. Douglas Drossman and Johannah Ruddy of the Rome Foundation return to share their expertise in effective patient-provider communications. They explain why it’s important for patients to clearly describe their symptoms and how patients can communicate with their healthcare providers even when the topic seems embarrassing. This episode also features expert tips on how patients can start the conversation with their healthcare providers about treatment options and alternatives for symptom relief when the patient feels the current treatment plan is not working.
April 20, 2022
How The Low FODMAP Diet May Improve Your IBS Symptoms
Registered Dietitian Emily Haller explains the 3 phases of the Low FODMAP diet and how it may help patients to manage their IBS symptoms by identifying specific foods that are more likely to trigger those symptoms. Emily also details the importance of working with a registered dietitian to replace trigger foods with alternatives to still maintain a healthy and nutrient dense diet, which she lays out in her 3-part course available for purchase on education.giondemand.com.
April 20, 2022
IBD/IBS Overlap: What Patients Need To Know
Some people with Crohn’s disease or ulcerative colitis can also experience symptoms common in irritable bowel syndrome (IBS) like gas, bloating, constipation, or abdominal pain. This episode aims to help patients understand the overlap between inflammatory bowel disease (IBD) and IBS from both physician and patient perspective. Dr. Katie A. Dunleavy from the Mayo Clinic in Rochester, MN, joins us to explain how and why the medical components of IBD and IBS can cross paths and the importance of a multidisciplinary approach to treatment, which includes pharmacological, dietary, behavioral health and other interventions. We’ll hear first-hand from Tina Aswani Omprakash, Patient Thought Leader & Founder of Own Your Crohn’s, who shares her personal health journey and offers tips for communicating with healthcare providers and living with a chronic illness. Johannah Ruddy, COO and Executive Director of The Rome Foundation, and co-founder of Tuesday Night IBS, shares her patient perspective and highlights the role of cognitive behavioral therapy.
Listen to our
latest Podcast!